COPD and Pneumonia Study (CAP)plus
COPD and Pneumonia Study (CAP)
STUDY COMPLETED and REPORTED
Did you know that you have a six to eight times greater risk of developing pneumonia if you have COPD?
Since COPD patients are at greater risk for developing pneumonia, we wanted to better understand the impact pneumonia has on the lives of our COPD community. Understanding the burden of pneumonia on the COPD community is important to help inform public health and prevention measures. Help us understand the burden of community acquired pneumonia by joining the online COPD and Pneumonia (CAP) study that was conducted through the COPD Patient-Powered Research Network (COPD PPRN).
This was the first completed study using the COPD PPRN platform which provided proof of concept for using this COPD360 Registry for surveys
The objectives of this study were to
-
assess the symptom burden of CAP
-
report time to symptom recovery
-
assess the impact of CAP on daily activities from the COPD patient perspective
The study surveyed nearly 500 individuals with COPD who had also recently received a Community Acquired Pneumonia (CAP) diagnosis, and concluded that individuals with COPD suffering from CAP will miss an average of 21 days from work with an additional 14 days required to return to “usual” job performance, will be impaired from normal activities for more than 30 days and experience weeks of lingering symptoms.
The results show that all the COPD-CAP-diagnosed participants experienced multiple symptoms including cough, breathlessness, and fatigue, often requiring weeks to recover and resulting in missing work and participation in usual activities. Over 84% reported requiring assistance from family and friends. The symptom and resulting burden were greater and lasted for a longer period than reported in the general community of CAP diagnosed individuals without COPD accessed in previous CAP studies.
Conclusion:
CAP causes a major burden in individuals with COPD their families and caregivers and it is important to ensure CAP prevention strategies including smoking cessation support and immunizations.
The results were reported in Pasquale CB, Vietri J, Choate R, et al. Patient-reported consequences of community-acquired pneumonia in patients with chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis. 2019; 6(2): 132-144.
A link to the publication: http://doi.org/10.15326/jcopdf.6.2.2018.0144
The CAP study was funded and sponsored by Pfizer and operationalized by the COPD Foundation through the PPRN.
The PArTNER Model Study - 2014-2019plus
The PArTNER Model Study - 2014-2019
STUDY COMPLETED and REPORTED
PATient Navigator to rEduce Readmissions (PArTNER)
PArTNER is a transitional care model for Minority-Serving Institutions (MSIs) that aims to increase support to patients and caregivers at the hospital through their transition home.
The design of the PArTNER study ClinicalTrials.gov Identifier: NCT02114515 is described in Prieto-Centurion et al Contemporary Clinical Trials Communications 2019.
The study was funded by a grant from Patient-Centered Outcomes Research Institute (PCORI)
THE PROBLEM
Often, there are gaps in the discharge process when a patient is transitioning from the hospital to home.
The patient sometimes serves as the only bridge between the hospital and home, while they are still recovering. This puts patients at risk during the transition of care. It can also cause extra stress for the patient and their caregiver.
Transitions of care without the PArTNER model:

When patients have limited resources, the gap can be even bigger
This problem was felt by patients + caregivers at an Illinois Minority-Serving Institution (MSI). Researchers talked to patients and caregivers from a MSI in Illinois about their hospital experiences. They said they wanted more support while in the hospital and once they were back at home. They also said they felt anxious about taking care of themselves after leaving the hospital.
"When I was diagnosed with CHF and COPD, I didn’t get no good talking to, you know, this is what to do now, this is what you need to change and stuff. You know, they just tell us, diagnose us with stuff. I be getting to think I’m a guinea pig"
Study Objectives
- To conduct a pragmatic clinical effectiveness trial comparing a multi-faceted, stakeholder-supported Navigator intervention versus usual care on the experience of hospital-to-home care transitions in patients hospitalized with heart failure, pneumonia, chronic obstructive pulmonary disease, myocardial infarction, or sickle cell disease;
- To examine the effectiveness of the Navigator intervention in patient subgroups;
- To understand the barriers and facilitators of successfully implementing the Navigator intervention across patient populations
MODEL DESIGN
With PArTNER, there are two added supports that strengthen the bridge between the hospital and home—the patient navigator and the peer coach.
Transitions of care with the PArTNER model:

The PArTNER model has multiple components.
The patient navigator visits the patient in the hospital at least once to assess for + address any health-related social needs like housing, transportation, food or utilities.

The patient navigator visits the patient at hospital discharge to go over discharge instructions and introduces them to their peer coach over the phone

The patient navigator visits the patient at home 1-3 days after hospital discharge to review discharge instructions and provide support to address any health-related social needs.

The peer coach calls the patients 5 times over the next two months to review discharge instructions and provide support to address any health-related social needs.

For more detail download the one-page PArTNER guide.
PARTICIPANT SNAPSHOT
The PArTNER model was tested in 1,029 patients hospitalized for heart failure, myocardial infarction, pneumonia, COPD or sickle cell disease at a MSI in Illinois.
On average, characteristics of the PArTNER patient population at a MSI:
- 50 years of age
- 82% of participants were Black
- 55% were women
- 50% had a high school degree or less
- 50% had annual household income less than $15,000
- had 3 hospitalizations in the past year
- 25% stated that the Emergency Department is their main place for medical care
The Study Report was published in 2018
Full findings from this pragmatic, clinical effectiveness trial testing the PArTNER model, can be found here.
STAFF + PARTNER
The PArTNER team would like to thank the patient navigators and peer coaches for their devoted care and support of the PArTNER participants.
The PArTNER team would also like to thank:
- The University of Illinois at Chicago PArTNER study staff
- The PArTNER Steering Committee members
- The PArTNER External Advisory Board members
- The PArTNER Principle Investigators and Co-Investigators

For more information, contact:
PArTNER@uic.edu
Population Health Sciences Program
University of Illinois at Chicago
PCP Needs Assessmentplus
PCP Needs Assessment
In 2007, the COPD Foundation jointly conducted the Primary Care Physician Needs Assessment with Outcomes, Inc. to evaluate the primary care patterns in outpatient COPD management, and to identify aspects of COPD care that should be targeted by educational initiatives.
Below you’ll find the key findings from this study. You may also access the full report here.
Key Findings
Physicians want more education on COPD management.
- It was found that 61.1% of Primary Care Physicians (PCPs) considered their recent COPD education exposure inadequate for their needs.
Physicians value clinical practice guidelines to help guide clinical practice, but have low awareness of COPD-specific guidelines.
- According to 64.4% of PCPs, clinical practice guidelines are the most important tool used in helping them provide optimal patient care.
- 44.9% of PCPs are unaware of clinical practice guidelines.
Spirometry poses significant challenges to PCPs since it’s the primary tool for confirming and staging COPD.
- 38.6% of PCPs lack spirometry in their practice. Of those with spirometry available, a third (35.6%) do not use it routinely.
- 64.8% of PCPs know how to use simple spirometry parameters to diagnose and stage COPD.
Physicians underutilize optimal bronchodilator therapies in patients with COPD, and over-utilize therapies with significant potential for adverse effects.
- Long-acting bronchodilators are recommended as first line therapy to control persistent COPD symptoms, but are not the drug of choice for physicians. In a patient with moderate-to-severe COPD who has not responded to initial therapy, only 36% appropriately chose a long-acting bronchodilator. According to guidelines, severe COPD should be treated with LABAs and steroids–particularly if there are exacerbations. Another problem here relates to the overlap between asthma and COPD, which can be substantial.
- Physicians often use inhaled steroids inappropriately in COPD patients, despite their significant risk for adverse effects. Given a spirometry-confirmed diagnosis of COPD, inhaled corticosteroids were chosen as initial therapy by 30.1% of physicians. This may be the appropriate therapy in patients who have asthma and COPD overlap.
The biggest obstacles to optimal COPD management in primary care were identified as the challenge of recognizing patients with early COPD and limited educational resources for newly diagnosed patients.
Resources
As a result of this study, the COPD Foundation has developed educational programs to address the specific gaps.
The PELICAN Studyplus

The PELICAN Study
PEer-Led o2 Info-line for patients and CAregivers (PELICAN)
The collaborative PELICAN study tested whether an O2 infoline for patients and caregivers will increase supplemental oxygen adherence and improve health in people with COPD. ClinicalTrials.gov identifier NCT02098369
STUDY COMPLETED and REPORTED
The problem
There are 3 interventions that save lives in people with COPD...
- Supplemental oxygen for resting hypoxemia
- Intensive smoking cessation interventions
- Non-invasive ventilation for COPD exacerbations
…but adherence to supplemental oxygen can be low.
- “I’m embarrassed to use my oxygen tank.”
- “I don’t think it works—I still get short of breath.”
- “The doctor sends you home on O2, you don’t know you’ll be on it the rest of your life.”
Study design
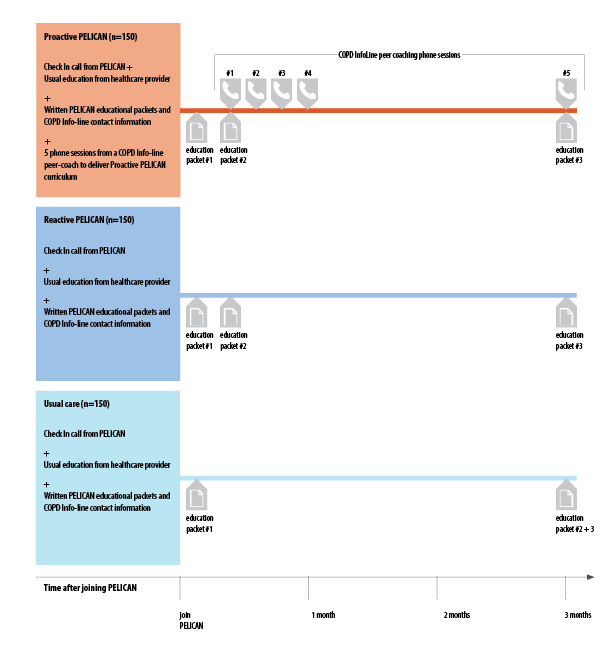
PELICAN is testing a care model that combines written self-management education materials and peer coaching phone sessions from the COPD InfoLine. Over 500 adult patients with a diagnosis of COPD and a prescription for home oxygen were randomized to one of three self-management groups--Proactive PELICAN, Reactive PELICAN, or usual care.
Participant snapshot
PELICAN enrolled over 500 participants with a diagnosis of COPD and a prescription for home oxygen.
- Over half of participants were more than 60 years old. Over 80% had used supplemental oxygen for at least 12 months.
- Nearly all patients used a stationary oxygen concentrator plus at least one other piece of oxygen equipment to use outside the home. Oxygen tanks and portable oxygen concentrators were the two most common pieces of oxygen equipment.
- About half of the participants had been hospitalized in the past 12 months.
Results have been reported in Krishnan J, Casaburi R, Cerreta S., et al. 2018. Using Phone-Based Peer Health Coaching to Improve Home Oxygen Use and Health in Patients with Chronic Obstructive Pulmonary Disease—The PELICAN Study. Washington, DC: Patient-Centered Outcomes Research Institute (PCORI) (Link to the final study report) and presented at the American Thoracic Society Conference in 2017 and 2018
Staff + partners
COPD Foundation InfoLine associates + leadershipplus
- Karen Anzalone
- Pam DeNardo
- Tim Deuby
- Ken Ellis
- Shelia Favazza
- Marilyn Hyatt
- Shirley Lawson
- Linda Mullin
- Sal Puccio
- Dugan Reed
- Jamie Sullivan
- John Walsh
- Linda Walsh
University of Illinois at Chicago study staffplus
- Jennifer Buenrostro
- Nina Bracken
- Crystal Cannon
- Jan Cotton
- Jessica Dudley
- Alexander Frye
- Vanessa Gonzalez
- Maciej Grabarek
- Sai Dheeraj Illendula
- Jerry Krishnan
- John Linnell
- Kyle Maggio
- Lourdes Norwick
External advising committeeplus
- Joel J. Africk Respiratory Health Association
- Rino Aldrighetti Pulmonary Hypertension Association
- Linda Arnold Patient
- Teresa Barnes Coalition for Pulmonary Fibrosis
- Helen Nichols Patient
- Thomas Kallstrom American Association for Respiratory Care
- Joseph Lewarski Drive Medical-DeVilbiss Healthcare
- Joseph Morrison Caregiver
- Jim Nelson Patient
Medical + scientific teamplus
- Richard Casaburi LA BioMed Research Institute / Harbor UCLA Medical Center
- Scott Cerretta COPD Foundation
- Kristen Holm National Jewish Health
- Jerry Krishnan University of Illinois at Chicago
- Janos Porszasz LA BioMed Research Institute / Harbor UCLA Medical Center
- Valentin Prieto-Centurion University of Illinois at Chicago
- Robert Sandhaus AlphaNet
- Jamie Sullivan COPD Foundation
Partnersplus
Co-Morbidities Surveyplus
Co-Morbidities Survey
The results of the study were included in Barr, R. G., Celli, B. R., Mannino, D. M., Petty, T., Rennard, S. I., Sciurba, F. C., Stoller, J. K., Thomashow, B. M., & Turino, G. M. (2009). Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. The American journal of medicine, 122(4), 348–355. https://doi.org/10.1016/j.amjmed.2008.09.042
In 2006 at the American Thoracic Society’s International Conference in San Diego, the COPD Foundation presented the results of the survey it took on COPD and co-morbidities.
Dr. Byron Thomashow and John W. Walsh presented the results of a phone survey conducted to 1,003 individuals, and 2,029 online surveys completed by individuals with COPD.
The goal of this survey was to study the incidence of co-morbid diseases, and impact on care received of individuals diagnosed with COPD–a topic seldom studied in the past. The survey instrument had over 75 questions, and addressed conditions such as diabetes, osteoporosis, depression, heart disease, and stroke, among others.
The results of the study indicated that co-morbidities are extremely common in the COPD community, and add significant complexity and cost of COPD care. The survey also suggested that despite significant symptoms, limitations, and health care utilization, surveyed COPD patients appear to be receiving less than maximal medical COPD therapy yet seem remarkably satisfied with the level of care. Those better connected to national COPD organizations appear to receive COPD care closer to suggested guidelines.
Over 81% percent of COPD patients in the household sample described having over 6 co-morbid conditions, as compared to 69% in organizational sample.
The breakdown revealed that 19% of the household sample reported 1 to 5 co-morbidities as compared 30% of the organizational sample, while 47% reported 6-10 co-morbidities in the household sample as compared to 53% of the organization sample.
For those reporting 11-15 co-morbidities, over one-fourth (27%) of the household sample reported this number, while only 14% of the organization sample reported 11 to 15 additional illnesses.
Finally, 7% of the household sample reported over 16 co-morbidities while only 2% of the organization sample reported this number.
The higher number of co-morbidities in the household sample corresponds to their worst health status. This greater number of co-morbidities also correlates to the larger number of pills taken daily as reported earlier: 59% of individuals in the household sample reported taking over 5 prescription medication per day compared to 48% in the organizational sample.
The study found that the majority despite preconceptions, COPD affected more women than men; in both groups, female respondents were more prevalent with 58% of household respondents being female as compared to 64% of organization respondents. Thus, overall 38% of survey respondents were male with 62% being female.